SBAR method of Communication
SBAR is a standardized way of communicating with other healthcare givers. It promotes patient safety because it helps physicians and nurses communicate with each other. Staff and physicians can use SBAR to share what information is important about a patient. It improves efficiency because this standardized form of communication helps caregivers speak about patients in a concise and complete way. It is also mandated by the Joint Commision on Accrediation of Hospital Organization which has added to Goal 2 in the 2007 Patient Safety Goals. The additional statement (2e) reads, “Implement a standardized approach to “hand off” communications, including an opportunity to ask and respond to questions.”
SBAR is an acronym that stands for:
Situation
Background
Assessment
Recommendation
Using SBAR, patient reports are more accurate, efficient, and consistent enterprise-wide. This simple, yet highly effective communication technique can be used when:
-A nurse is calling a physician
-Nurses are handing off patients to one another
-Nurses are transferring patients to other facilities or to other levels of care
SBAR promotes better communication. In most cases nurses and physicians communicate in very different ways. Nurses are taught to report in narrative form, providing all details known about the patient. Physicians are taught to communicate in using brief “bullet points” that provide key information to the listener.
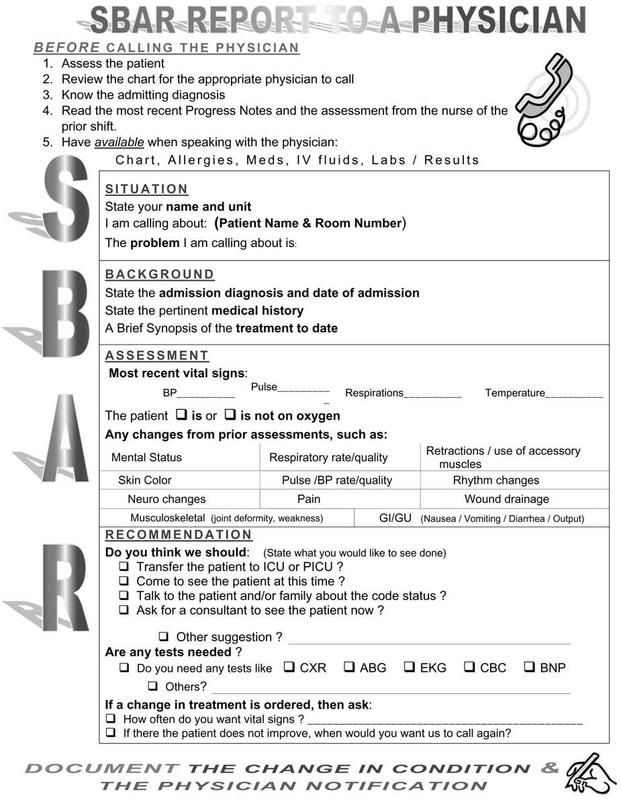
This is the form on how Nurse's should report to a physician
 Here is an example of how to use the template:
Here is an example of how to use the template:
Dr. Jones, this is Jedz Cutie RN, I am calling from PBSN Hospital about your patient Mr. D. Bitteroot.
Situation: Here's the situation: Mr. Bitteroot is having increasing dyspnea and is complaining of chest pain.
Background: The supporting background information is that he had a total knee replacement two days ago. About two hours ago he began complaining of chest pain. His pulse is 120 and his blood pressure is 128/54. He is restless and short of breath
Assessment: My assessment of the situation is that he may be having a cardiac event or a pulmonary embolism.
Recommendation: I recommend that you see him immediately and that we start him on 02 stat.
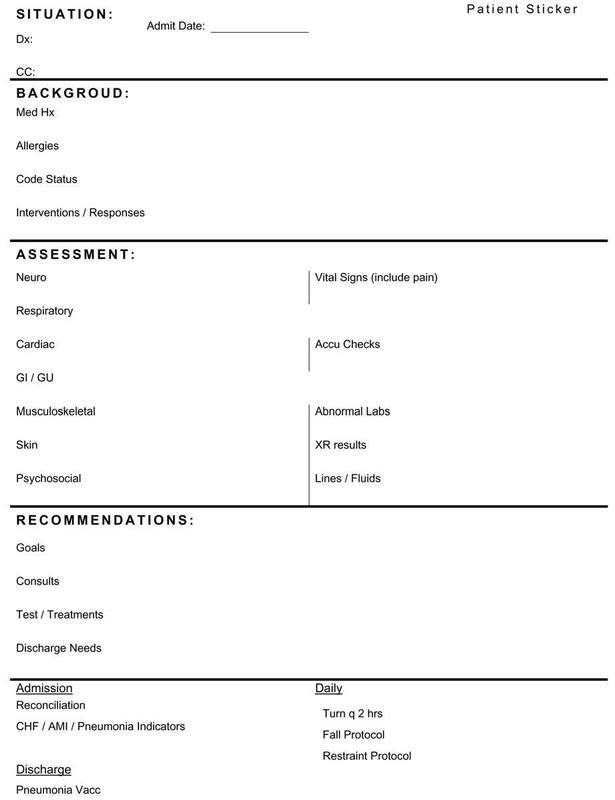
Another form that is used is the Hand-off form which can be used for exchange of shift report used by nurse to nurse communication.
REFERENCE: Kathleen M. Haig, R.N., Staci Sutton, R.N., John Whittington, M.D. "SBAR: A Shared Mental Model for Improving Communication Between Clinicians" Joint Commision on Quality and Patient Safety www.jcipatientsafety.org/fpdf/psp/SBAR.pdf (Last Accessed, May 25, 2008)















some comments lng re the example:
I think it should be more comprehensive especially the assessment, for pt having dyspnea o2 sat should be checked as well as increasing restlessness to know if the pt is a candidate for intubation; another thing is breath sounds should also be checked prior to informing the doctor. another is the quality of chest pain.
Remmeber we can't diagnose a cardiac event or pulmonary embolism, without prior exams and assessment.
It is a protocol to hook pt on 02 at 2lpm (safest) when having dyspnea, we don't have to recommend it (that should be done initially. What we should recommend is if we should shift the cannula to a facemask at how many lpm, if we're going to have stat ABG, trop T, CKMB, and if we could give isordil for chest pain( if its not muscle pain).
referrals should be done on the first sign of dyspnea not after 2 hours. ok!
Posted by Anonymous |
12:05 AM
Anonymous |
12:05 AM
You must got this wrong. You are not referring to a resident. In the states, You will have attending physicians or consultants, they are not on the hospital, you will just CALL THEM ON THE PHONE, imagine if you will include so much unecessary informations, your doctor will hang up on you.
Another thing, its ASSESSMENT, not diagnosis. You will say "Doctor I think our patient is having a cardiac event or pulmunary embolism" You will do this because the Attending Physician cannot see the patient. This it is done in the US. Nurses are not just limited to VS and there are much expected of you. So one tip when you go there, do not act like that.
Protocol will depend on the hospital you are working on, thats why its called PROTOCOL. Of course in cases of dyspnea, you can hook the patient to O2, any "nurse" should know that. It was not stated in the example that, It was not done prior to the referral. it was just so stated so that the doctor knows what u did and if he disapprove, you can stop 02 therapy.
You said u want to shift to a face mask, but int the said situation, the patient wast just dyspniec not GASPING.
Imagine starting CPK-MB, its onsent is about 4 hours and peak after 12 hours, and you draw blood immediately, so do you think u will have a result. Wrong recommendation. Same with troponin. So Imagine giving a patient a medication you are not sure, ISDN will help angina, but not MI. worng recommendation. For pulmunary embolism V/Q scan is recommended but it will take preparations. So lets not over ride our boundaries and let the physician do the ordering of such diagnostics and lab work up. thats is why you are refferring to him.
If you will refer a patient just for dyspnea, and no other pertinent observation... how can you give much information? remember YOU ARE NOT calling a RESIDENT, this is the ATTENDING PHYSICIAn and you are talking on the PHONE
Posted by Jeddah |
10:45 AM
Jeddah |
10:45 AM
so u mean, there is a great difference on referrals with residents and consultants? well, i don't think so, they're both certified doctors and referrals should be done the same way. i believe doctors will not hang up on you with my kind of referral, it will just decrease those things that that the doctor will surely ask. besides your giving him a subjective data without even taking an objective one (re dyspnea).
Come on! pulmonary embolism and cardiac event (which one), are medical diagnosis, those are not assessment. show me a book! you may say after your assessment that you are considering which cardiac event and PE.
dyspneic means difficulty of breathing, you did'nt even mention how severe it is, so i considered stat ABG.
Why not do CKMB, or tropT, trop I? yeah, i believe with the "peaks" that you've mention, but with your assessment of the so called cardiac event, we need something to rule it out. I did not mean immediately, ABG is the only stat that i've mentioned.
Another thing is, i'm not doing the ordering i'm just giving suggestions. i know my limits for sure.
by the way, how did you know that it is not angina? you did'nt even assessed, having a cardiac event is a broad category, it may be MI, angina, arrhythmias, it may even be asystole. Watch your terms.
Posted by Anonymous |
9:50 AM
Anonymous |
9:50 AM